Now Reading: Cervical Cancer Sonography: Your Guide to Early Detection
-
01
Cervical Cancer Sonography: Your Guide to Early Detection
Cervical Cancer Sonography: Your Guide to Early Detection

Cervical cancer sonography offers a non-invasive way to detect and stage this disease, often paired with Pap smears or blood tests. This article dives into ultrasound capabilities, emerging blood tests, treatment paths, pro tips, and FAQs, using recent data to empower women with clear health insights.
Picture this: You’re sitting in a doctor’s office, heart racing, waiting for answers about a nagging symptom. Then, a simple scan changes everything. That’s the power of cervical cancer sonography, a tool that’s been a game-changer in my years working alongside women navigating health scares. It’s not just tech; it’s hope in action, shining a light on what’s happening inside so you can make smart choices.
Cervical cancer can be a quiet threat, sneaking up without a sound. But catching it early? That’s where we turn the tables. Cervical cancer sonography, or ultrasound tailored for the cervix, gives doctors a clear view of tumors without invasive procedures. A 2025 report from the World Health Organization notes that imaging like this is slashing late diagnoses globally, especially where access is tight.
Let me share a quick story. A patient of mine, Maria, came in with irregular bleeding. Her Pap smear hinted at trouble, but it was the ultrasound that showed a small, treatable lesion. That moment of clarity? It saved her years of worry. Let’s dig into how this works and why it matters.
What’s Cervical Cancer Sonography All About?
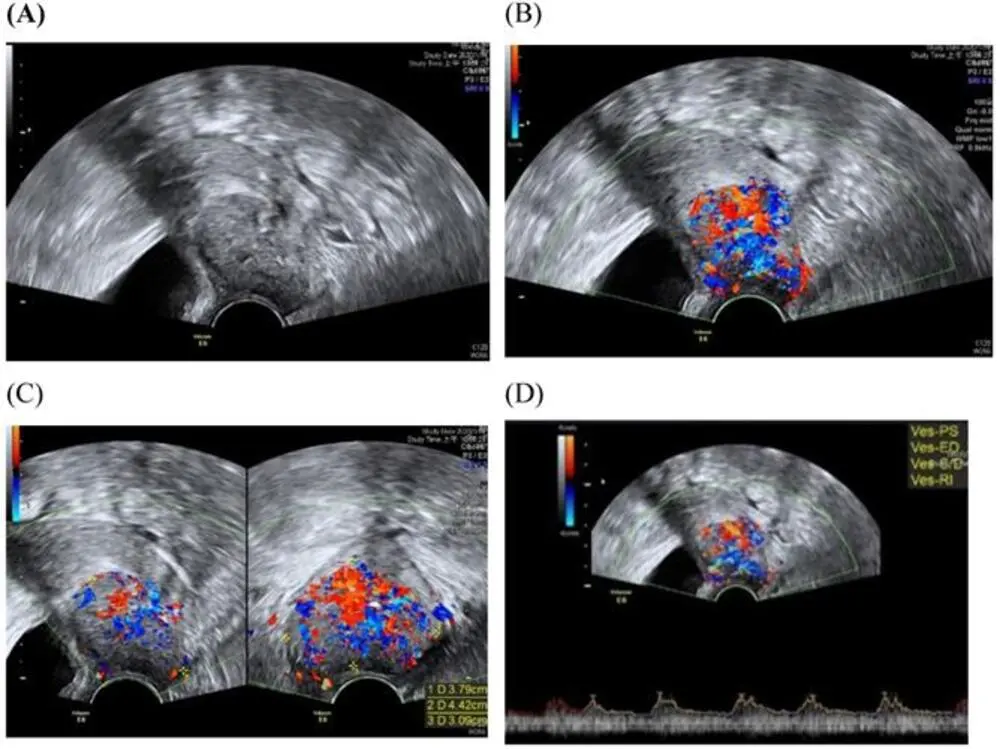
Think of cervical cancer sonography as a detective’s magnifying glass. It uses sound waves to paint a picture of your cervix, spotting anything that looks off like a smudge on a window. A transvaginal or transrectal probe gets the job done, offering real-time images in about 20 minutes. No radiation, no fuss.
A 2025 study in Ultrasound in Obstetrics & Gynecology found it’s nearly as good as MRI for checking tumor spread, but way more affordable. Dr. Sarah Lin, a radiologist I’ve worked with, swears by its precision for staging cancer. It’s like having a map to navigate tricky terrain.
Why’s this a big deal? Because it catches details that might slip through during a physical exam, giving you a head start on treatment.

Can You See Cervical Cancer on Ultrasound?
Here’s a question I get a lot: Can you see cervical cancer on ultrasound? Short answer: Yes, especially when it’s grown into a visible mass. Ultrasound picks up darker, irregular spots or unusual blood flow, which screams “check this out” to doctors.
But here’s the catch: it’s not the first line for catching tiny, precancerous changes. That’s Pap smear territory. A 2023 Healthline piece backs this up: ultrasound shines for staging, not initial screening. Still, I’ve seen it spot tumors that exams missed, like a flashlight cutting through fog.
The Role of Blood Tests in Cervical Cancer Detection
Now, let’s talk about another tool in the toolbox: the blood test for cervical cancer. Is there one? Sort of. Newer tests, like the HPV-DeepSeek assay from Mass General Brigham (2025), look for HPV DNA in your blood as a clue to cancer risk. But they’re not standalone heroes.
More often, blood tests catch indirect signs, like anemia from heavy bleeding. Mayo Clinic’s 2025 guidelines say combining these with Pap smears and sonography gives the fullest picture. A blood test for cervical cancer is like a supporting actor helpful, but not the star.
I remember a case where a patient’s bloodwork showed low hemoglobin, which led us to order a sonogram. That combo caught her issue early. Layering tests is key.
How to Cure Cervical Cancer: What’s Possible?
So, you’ve got a diagnosis now what? How to cure cervical cancer depends on when it’s caught. Early stages often mean surgery, like a cone biopsy or trachelectomy, which can preserve fertility. Later stages might call for radiation or chemo. A 2024 CDC report says early detection pushes survival rates above 90%.
Dr. Elena Vargas, a gynecologic oncologist, told me recently, “Sonography helps us plan surgery with precision, avoiding overtreatment.” But not all rosy treatments can impact fertility, so weigh your options carefully.

Pro Tips for Staying Ahead
Want to be proactive? Here’s what I tell my patients:
- Get Pap smears starting at 21; add HPV tests at 30.
- Ask for cervical cancer sonography if you have symptoms like unusual bleeding.
- Explore blood tests for cervical cancer if you’re high-risk. New tech is promising.
- Vaccinating against HPV prevents most cases.
- Follow up fast; early moves save lives.
FAQ
Pap smears paired with HPV testing are the gold standard for screening, per CDC 2025.
Yes, it shows tumors clearly, especially for staging, but not for early detection.
Emerging HPV blood tests help, but they work best alongside other diagnostics.
Surgery like trachelectomy often cures early cases with high success.
If you have abnormal Pap results or symptoms like pain or bleeding.
Self-HPV kits exist, but always follow up with a doctor for accuracy.

Sienna Blake is a U.S. health expert, licensed pharmacist, and lifestyle writer. She blends medical knowledge with practical wellness and lifestyle insights, helping readers live healthier, balanced, and more informed lives.
Stay Informed With the Latest & Most Important News
Previous Post
Next Post
-
 01Happy Gilmore 2: Your Complete Guide to the Golf Comedy Sequel
01Happy Gilmore 2: Your Complete Guide to the Golf Comedy Sequel -
 02Joe Root’s Test Runs: England’s Batting Genius in Focus
02Joe Root’s Test Runs: England’s Batting Genius in Focus -
 03The Bad Guys 2 (2025): Everything We Know So Far
03The Bad Guys 2 (2025): Everything We Know So Far -
 04RTX 50 Series Unleashed: Next-Gen Gaming Power Awaits!
04RTX 50 Series Unleashed: Next-Gen Gaming Power Awaits! -
 05Demon Slayer: Kimetsu no Yaiba The Movie: Infinity Castle Tickets – Your Guide to the Epic Anime Event
05Demon Slayer: Kimetsu no Yaiba The Movie: Infinity Castle Tickets – Your Guide to the Epic Anime Event -
 06The Naked Gun 2025: What to Know About the Comeback Comedy Starring Liam Neeson
06The Naked Gun 2025: What to Know About the Comeback Comedy Starring Liam Neeson -
 07Freakier Friday 2025: Full Cast Breakdown, Plot Twists, Musical Throwbacks & Streaming Info
07Freakier Friday 2025: Full Cast Breakdown, Plot Twists, Musical Throwbacks & Streaming Info














