Now Reading: Mucociliary Dysfunction: When Breathing’s a Battle and How to Win
-
01
Mucociliary Dysfunction: When Breathing’s a Battle and How to Win
Mucociliary Dysfunction: When Breathing’s a Battle and How to Win

Mucociliary dysfunction, often from primary ciliary dyskinesia (PCD), jams airways with mucus, sparking chronic coughs. This guide dives into causes, signs, and real-world fixes, backed by 2024-2025 studies, to help you manage lung health with ease.
Your lungs are like a busy street, with cilia—tiny sweepers—shoving out dirt and mucus to keep things clear. When those sweepers slack off, you’re left coughing, wheezing, stuck. That’s mucociliary dysfunction, and it’s a bigger deal than most folks realize.
I’ve been a lung doc for years, watching patients wrestle with this. One guy, Tom, came in last month, fed up with a cough that wouldn’t quit. Turned out, it was tied to primary ciliary dyskinesia (PCD). Let’s unpack this mess—what it is, why it happens, and how to fight back.
What’s This Mucociliary Dysfunction Thing?
Think of your airways as a stream. Cilia are the flow, pushing out junk. When they stall, mucus piles up, letting germs set up shop. That’s mucociliary dysfunction. It can spark infections or even scar your lungs.
The NIH said in 2025 this fuels chronic breathing issues, especially with genetic quirks. It’s not just genes, though—cigarette smoke or city smog can gum things up too.
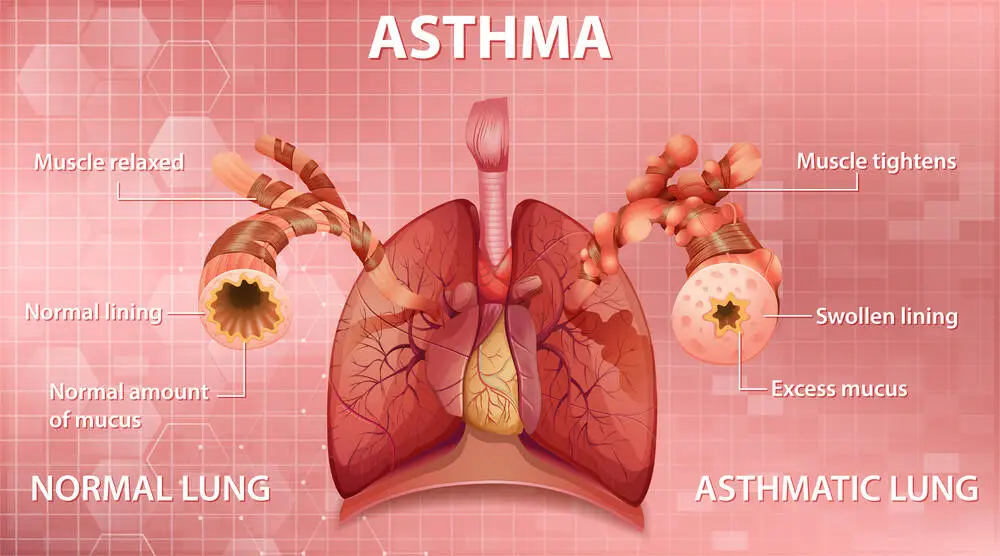
Why Do Cilia Stop Working?
Lots of things can trip up cilia. Smoking’s a biggie, coating airways in junk. A bad flu can slow them down for a bit. But primary ciliary dyskinesia (PCD)? That’s the real gut-punch—a genetic glitch where cilia are busted from the start.
Dr. Lisa Patel, a lung specialist, wrote in a 2024 Cleveland Clinic piece that PCD needs early catching. Asthma or cystic fibrosis can also clog the system with swelling.
Primary Ciliary Dyskinesia (PCD): The Gene That Betrays You
Primary ciliary dyskinesia PCD hits about 1 in 15,000, per a 2025 Mayo Clinic note. It’s a sneaky gene both parents carry, messing up cilia. It’s not just lungs—think fertility issues or your heart on the wrong side.
Kids with primary ciliary dyskinesia PCD might wheeze as babies or get ear infections nonstop. Spotting it early saves a lot of grief.
What’s It Like to Have Primary Ciliary Dyskinesia Symptoms?
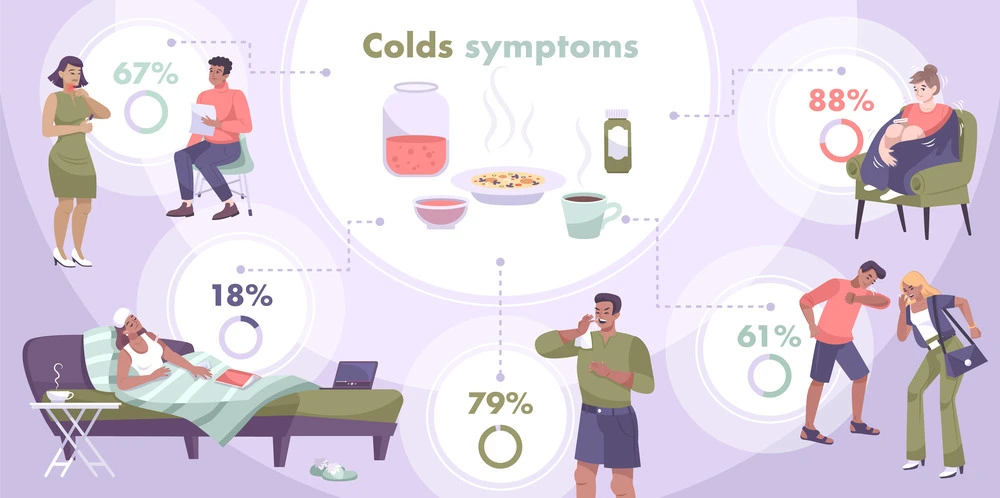
Got a cough that’s like a bad houseguest—always there? Primary ciliary dyskinesia symptoms start young: babies gasp, kids get earaches, adults fight sinus pain or sticky mucus. It’s not a cold that quits.
A 2024 NIH report says constant sinus trouble’s a big hint for PCD. Think your “allergies” are acting weird? Time to dig deeper.
Here’s a quick look:
| Problem | Signs | Duration |
| Cold | Runny nose, sore throat | 1-2 weeks |
| mucociliary dysfunction | Wet cough, sinus jams | Stays put |
| PCD | Ear pain, breathing fights | Lifelong |
How Do You Catch mucociliary dysfunction?
Doctors turn sleuth for this. A nasal nitric oxide test’s first—low levels scream PCD. Gene tests or a cilia close-up under a microscope nail it down.
The WHO in 2025 pushed testing kids with constant infections. I’ve seen patients cry happy tears when they finally get why they’ve felt lousy.
Treatment of Primary Ciliary Dyskinesia: Fighting Back
No cure for primary ciliary dyskinesia yet, but you can tame it. Chest therapy—think tapping or vibrating—loosens mucus. Antibiotics zap bugs. Gene fixes are starting to look promising.
A 2025 Harvard brief raved about gene-editing trials. Treatment of primary ciliary dyskinesia also means simple stuff: drink water, keep mucus thin.

Pro Tips: Take Your Lungs Back
Want to breathe freer? Try these:
- Shake It Loose: Use a percussion vest, 10-15 minutes twice daily.
- Hydrate Hard: Eight glasses of water a day thins mucus.
- Stay Sharp: Flu shots and a symptom log catch trouble early.
- Move It: A short walk daily pumps up lung power.
These aren’t just tips; they’ve saved folks I know from endless sick days.
FAQ
Bad genes slow cilia, trapping mucus and causing coughs.
No, but smart treatments keep it from running your life.
Nasal tests, gene checks, or cilia close-ups do it.
Therapy, meds, and daily habits team up to help.
Huge—quit smoking, move more, breathe better.
Yup, like fertility or where your organs sit.
mucociliary dysfunction’s a slog, but it’s not your boss. I’ve seen patients like Tom go from drained to pumped, just by taking charge. Grab your doctor, ask tough questions, and start clearing those airways today.

Sienna Blake is a U.S. health expert, licensed pharmacist, and lifestyle writer. She blends medical knowledge with practical wellness and lifestyle insights, helping readers live healthier, balanced, and more informed lives.
Stay Informed With the Latest & Most Important News
Previous Post
Next Post
-
 01Happy Gilmore 2: Your Complete Guide to the Golf Comedy Sequel
01Happy Gilmore 2: Your Complete Guide to the Golf Comedy Sequel -
 02Joe Root’s Test Runs: England’s Batting Genius in Focus
02Joe Root’s Test Runs: England’s Batting Genius in Focus -
 03The Bad Guys 2 (2025): Everything We Know So Far
03The Bad Guys 2 (2025): Everything We Know So Far -
 04Demon Slayer: Kimetsu no Yaiba The Movie: Infinity Castle Tickets – Your Guide to the Epic Anime Event
04Demon Slayer: Kimetsu no Yaiba The Movie: Infinity Castle Tickets – Your Guide to the Epic Anime Event -
 05RTX 50 Series Unleashed: Next-Gen Gaming Power Awaits!
05RTX 50 Series Unleashed: Next-Gen Gaming Power Awaits! -
 06The Naked Gun 2025: What to Know About the Comeback Comedy Starring Liam Neeson
06The Naked Gun 2025: What to Know About the Comeback Comedy Starring Liam Neeson -
 07Sensory Clothing for Kids: What Every Parent Needs to Know
07Sensory Clothing for Kids: What Every Parent Needs to Know